Are you sure it’s lactose intolerance and not delayed cow’s milk allergy?
10/10/2013 9:59:36 AM
A large number of parents I come across tell me their baby has lactose intolerance. Unfortunately, this may not be the case as lactose intolerance in babies is usually only secondary to another condition.
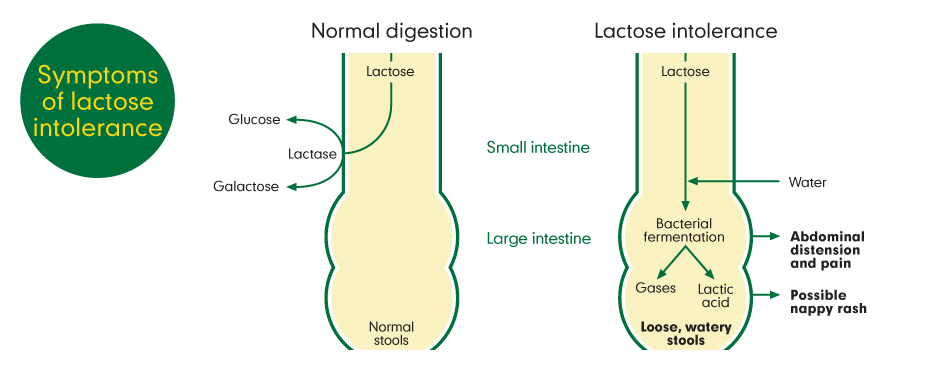
Lactose intolerance usually occurs after a stomach infection (gastroenteritis), which causes damage to the cells that produce the enzyme lactase in the small intestine. This enzyme digests lactose, the sugar found in breast milk, infant formula and cow’s milk. If there isn’t enough of the lactase enzyme, undigested lactose moves through the gut into the large intestine. Here, bacteria ferment the sugar to produce lactic acid and gases. These can cause abdominal distension and pain. Lactose and lactic acid attract water, so symptoms of loose, watery diarrhoea are usually present. It also makes the stools acidic and so can cause nappy rash.
Using a low lactose formula for 6-8 weeks helps the gut to recover and produce more lactase, and then your baby can tolerate normal formula again. If you are breast feeding, you can give your baby some lactase enzyme before, during and at the end of the feed. Cutting out dairy products from a breast feeding mum’s diet will not change the type or quantity of sugar in breast milk – the sugar in breast milk will only ever be lactose.
Many parents tell me they also had lactose intolerance as a child. However, there are only 2 forms of lactose intolerance that can be inherited:
i) Congenital lactose intolerance which is so rare most paediatricians will never see a case
ii) Primary lactose intolerance which doesn’t tend to cause symptoms until primary school age
If there is a family history of symptoms associated with milk; either breast milk, infant formula or cow’s milk, it is far more likely to be due to a delayed cow’s milk allergy (non-IgE mediated).
Immediate type reactions (IgE mediated) such as hives and facial swelling are much easier to identify and tend not to be confused with lactose intolerance.
If your baby has a cow’s milk allergy, it means their immune system is over-reacting to the proteins present in cow’s milk. In lactose intolerance, it is the sugar in the gut that is not digested properly, and the immune system is not involved.
Why can’t you test to see if it’s lactose intolerance or cow’s milk allergy?
Tests such as reducing substances and low pH in stools, or a hydrogen breath test will tell you whether your baby or child may be suffering from lactose intolerance, but it does not tell you whether the lactose intolerance is due to cow’s milk allergy.
Unfortunately there are no tests available to determine whether your baby or child has delayed cow’s milk allergy (reaction usually happens 2 hours or more after ingestion). Immediate reactions can be confirmed with a skin prick test or blood test. For delayed reactions, the suspected allergen (e.g. cow’s milk protein) has to be removed from the diet for a period of 2-6 weeks to see if the symptoms go away, and then it is put back in to see if the symptoms come back. This gives the diagnosis of delayed cow’s milk allergy. If you want to investigate this, please discuss with your GP or childrens health team. See my article on allergy testing – the right and wrong ways.
The confusing thing is that using a lactose free formula can improve the symptoms of loose stools, nappy rash, abdominal distension and pain. This is because you can get lactose intolerance due to gut inflammation (intestinal mucosal injury) caused by untreated cow’s milk allergy. Children under 2 years of age are very susceptible, due to
- the high sensitivity of their gut
- low reserve of lactase due to a small intestinal surface area
- large intake of milk and dairy products.
If you take out lactose, you are treating some of the symptoms, but you are not treating the underlying cause. Therefore your baby cannot tolerate a normal formula after the expected 6-8 week period, as the cow’s milk protein continues to cause gut inflammation and on-going lactose intolerance.
Unfortunately, there seems to be an increasing trend for lactose free formula to be prescribed as an alternative to soya formula, despite no recent history of gastroenteritis. This is likely to be due to a combination of cost, palatability and lack of understanding of the symptoms and management of cow’s milk allergy.
Soya formula is both cow’s milk protein and lactose free but is not recommended for babies under 6 months of age due to the presence of phytoestrogens, which may pose a risk to their long-term reproductive health. There is also a high risk of cross-reactivity between cow’s milk and soya in babies with gut allergy symptoms so that a number of these babies end up having to avoid both soya and cow’s milk products.
The following table of symptoms should help you identify whether your baby is more likely to have a cow’s milk allergy or lactose intolerance
| Symptoms of lactose intolerance |
Symptoms of cow’s milk allergy |
- loose, watery, frequent stools
- abdominal pain and distension
- excessive flatulence
- infantile colic
- nappy rash
|
- loose, watery, frequent stools
- abdominal pain and distension
- excessive flatulence
- infantile colic
- nappy rash
- mucousy, bloody or offensive stools
- constipation
- vomiting or gastro-oesophageal reflux
- poor weight gain
- food refusal
- eczema
- other atopic conditions such as hay fever, runny or congested nose, wheeze or cough, hives (urticaria) or swelling (angioedema), anaphylaxis
- family history of cow’s milk allergy
|
If you are concerned that your baby or child may have cow’s milk allergy, please seek advice from a health professional experienced in food allergy.
Further information is available from:
http://www.patient.co.uk/health/lactose-intolerance
Nottinghamshire Area Prescribing Committee (APC) have published two guidelines: http://www.nottsapc.nhs.uk/index.php/clinical-guidelines
1) Guidance on the diagnosis and management of lactose intolerance and prescription of low lactose infant formula (‘L’ for lactose)
• Patient information leaflet for the management of secondary lactose intolerance in Nottingham is also available.
2) Guidance on the diagnosis and management of cow’s milk allergy (‘C’ for cow’s milk)