Does my child have gastro-oesophageal reflux, cow’s milk allergy or both?
8/28/2015 12:03:09 PM
According to the new
NICE gastro-oesophageal reflux disease (GORD) guidelines for children1, there is not enough evidence to support the belief that non-IgE mediated cow’s milk allergy (CMA) is a cause of GORD. NICE have therefore recommended specific research to answer this question. But what do we do in the meantime?
 Symptoms of gastro-oesophageal reflux and cow’s milk allergy
Symptoms of gastro-oesophageal reflux and cow’s milk allergy
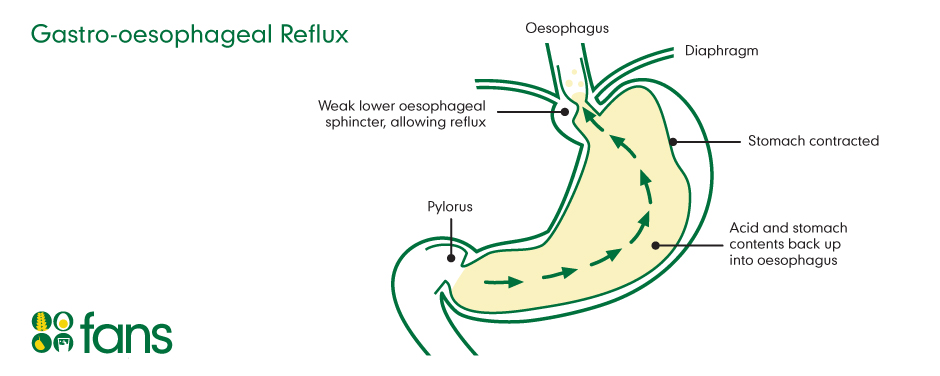
Gastro-oesophageal reflux is very common in young children, and many babies will happily vomit away. It only becomes a problem when it starts to cause significant pain and distress. However, non-IgE mediated cow’s milk allergy can also cause much pain and many of the symptoms are similar for both as shown in the table below:
| Gastro-oesophageal reflux disease (GORD) |
Non-IgE mediated cow’s milk allergy (CMA) |
| Recurrent vomiting (up to 2 hrs after feeding) |
Recurrent vomiting (up to 2 hrs after feeding) |
| Freq. & troublesome crying, irritability or back arching during or after feeding and feed refusal |
Freq. & troublesome crying, irritability or back arching during or after feeding and feed refusal |
| Dysphagia/ frequent choking after feed |
Dysphagia/ frequent choking after feed |
| Iron deficiency/ anaemia |
Iron deficiency/ anaemia |
| Faltering growth |
Faltering growth |
| Sleeping difficulties |
Sleeping difficulties |
| Reflux oesophagitis (inflammation of the oesophagus) |
Eosinophilic oesophagitis (not so common) |
| Stridor, hoarseness |
Stridor, hoarseness (tends to only occur in IgE mediated CMA i.e. immediate onset reactions) |
To work out whether your child is suffering from GORD, CMA or both, you need to look for symptoms that are different between the two.
Some of the key differences in symptoms are as follows:
| Gastro-oesophageal reflux disease (GORD) |
Non-IgE mediated cow’s milk allergy (CMA) |
| Epigastric pain/ heartburn |
Abdominal distension and pain |
| Sinusitis and recurrent ear infections (otitis media) |
Nasal congestion or runny nose, allergic shiners (black rings signifying congestion around the eyes) |
| More settled when held upright |
Positioning makes little difference to level of distress |
| Bronchitis (inflammation of the lungs), recurrent aspiration pneumonia & apnoea (rare) |
Atopic conditions e.g. eczema, rhinitis/ hayfever, wheeze/ asthma in either the child or family members increases likelihood of food allergy involvement |
| |
Projectile (forceful ) vomiting after feeds (rule out pyloric stenosis in infants < 2mths) |
| |
Diarrhoea or constipation, offensive/ explosive stools, mucus or blood in stools (rule out intussusception ) |
Cavataio and colleages (2000) suggest that cow’s milk allergy is present in up to 42% of children with GORD
2. According to Farahmand and colleagues (2011),
one third of their children with symptoms of GORD had cow’s milk allergy, suggesting that CMA can mimic or aggravate GORD
3.
In my experience, if your child is suffering from:
- other gut symptoms such as diarrhoea or constipation
- has atopic symptoms involving the skin such as eczema, rashes or the respiratory tract such as congestion, constant runny nose, wheeze or asthma,
they are likely to be suffering from non-IgE mediated cow’s milk allergy and it would be appropriate to try a 4 week cow’s milk exclusion trial first, in accordance with
NICE guidance on the diagnosis and assessment of children with food allergy4
If your child’s symptoms do not include the above combination, but match the symptoms listed for GORD, start with first line management recommendations for reflux disease.
First line treatment for GORD
NICE GORD guidelines recommend that breastfed babies receive a breastfeeding assessment with advice, and formula-fed babies are given advice on appropriate feed volumes and frequency of feeds
1.
Thickening milks
Following general feeding advice, NICE recommend that formula-fed babies are offered a trial of thickened formula first; either a specialist anti-reflux formula or addition of a thickener
such as carob bean gum i.e. Instant Carobel™ to the existing formula. This recommendation concurs
with the
clinical knowledge summary (CKS) of GORD in children5 which provides more practical based information.

Evidence suggests that thickened formulas may reduce vomiting in babies, but they do not reduce the number of reflux events. It is important to note that specialist anti-reflux formulas cannot be made up in accordance with the Department of Health guidance using water at 70
0C, as it will break down the thickener before it reaches the stomach, so it is essential that only one bottle is made up at a time, in accordance with the manufacturer’s instructions, to minimise risk of bacterial contamination.
If no benefit is observed, a further trial using alginate therapy i.e. Gaviscon Infant™ is recommended by NICE. However, this is also just a thickening agent, unlike alternative preparations of Gaviscon which contain an antacid. It should therefore not be used in conjunction with other thickeners, as this could over-thicken the stomach contents and risk causing blockages.

Gaviscon Infant is more difficult to use, as the number of sachets is restricted due to its high sodium content (6 doses /3 dual sachets a day). As a result, it can be difficult to divide the doses between all bottles, and being a thickener, it needs to be present in every bottle. However, it tends to thicken in the stomach in a similar way to the anti-reflux formula, so a faster teat should be sufficient. Instant Carobel thickens in the bottle and can continue to thicken, so it can take some practice to get the consistency right.
For
breast fed babies however, NICE only recommend a trial using alginate therapy, their feedback being that there is no evidence on use of alternative thickeners for this group of infants1. The CKS guidelines however, address this well and highlight that guidance from the manufacturer of Instant Carobel™ is available and their expert reviewers support a trial of this first, despite a lack of evidence to support its benefits
5.
Side effects: According to
NHS Choices medicine guide, abdominal distension is a side effect of Gaviscon Infant. However, it is commonly reported to me that trials of Gaviscon Infant in particular, but other thickeners too, can cause constipation. NICE replied that there have been no adverse events reported from thickening therapies. It is possible that this is more common in children with non-IgE mediated cow’s milk allergy, as this is the group of children that I am involved with. Further evidence is clearly needed.
Other first line practical management strategies6
- Avoid overfeeding your child and try smaller volumes more frequently if practical
- Careful winding during feeds and keep child upright for 20-30 minutes after a feed
- Avoid constipation, aiming for one bowel motion a day
- Recognise your child’s cues and respond early, to avoid excessive crying, which can bring on reflux
- Consider weaning a little earlier i.e. between 4-6 months, but never before 17 weeks of age
- Avoid giving your child juice and other acidic foods. For older children, see advice sheet on sensible eating for gastro-oesophageal reflux
- If unresponsive to first line measures, including feed thickeners, undergo an allergy focused clinical history to rule out possibility of cow’s milk allergy, in accordance with NICE4 . Check my website, to see if the online allergy assessment tool is up and running, or contact me to discuss http://foodallergynottingham.co.uk/
Undertaking a cow’s milk exclusion trial may resolve all of your child’s symptoms, although in some cases, all the symptoms resolve apart from ongoing vomiting and possible distress, which suggests that your child may be suffering from both GORD and CMA. In such cases, if looking to thicken the formula, a thickener such as Instant Carobel™ added to hypoallergenic formula is the only option, as would be used for breast milk.
Pharmacological treatment
If your child continues to suffer from unexplained feeding difficulties such as food refusal, gagging or choking, continues to be distressed and/ or may show faltering growth, NICE recommend that they should be considered for a 4 week trial on acid-suppressing drugs such as proton pump inhibitors e.g Omeprazole™ or H2 receptor antagaonists e.g. Ranitidine™.
You should speak to your GP, who is likely to refer your child to a paediatrician.
References
1. NICE (2015). Gastro-oesophageal reflux disease: recognition, diagnosis and management in children and young people.
NICE guideline. Published: 14 January 2015
2. Cavataio et al (2000). Milk-induced reflux in infants less than one year of age. J Pediatr Gastroenterol Nutr;
30 Suppl: S36-S44
3. Farahmand et al (2011). Cow’s milk allergy among children with gastro-oesophageal reflux disease. Gut and Liver;
5 (3): 298-301
4. NICE (2011). Food allergy in children and young people - Diagnosis and assessment of food allergy in children and young people in primary care and community settings
NICE clinical guideline 116.
5. NICE Clinical Knowledge Summaries (CKS) (2009).
GORD in children.
6. Sutphen (2001). Is it colic or is it gastro-oesophageal reflux? J Pediatr Gastro Nutr;
33 (2): 110-111
Further reading
Vandenplas,Y., Rudolph,C.D., Di Lorenzo,C. et al (2009) Pediatric gastroesophageal reflux clinical practice guidelines: joint recommendations of the North American Society of Pediatric Gastroenterology, Hepatology, and Nutrition and the European Society of Pediatric Gastroenterology, Hepatology, and Nutrition. Journal of Pediatric Gastroenterology and Nutrition 49(4), 498-574.
Onyeador et al (2014). Paediatric gastro-oesophageal reflux clinical practice guidelines. Arch Dis Child Educ Pract Ed; 99: 190-193